Despite being less known and often overlooked by the general public, bacteriophages have been evolving alongside bacteria and may have existed even before bacteria. The complexities of this natural evolution, combined with the artificial abuse of antibiotics, have led the scientific community to consider bacteriophages as a potential alternative to antibiotic drugs before it’s too late. The idea of using bacteriophages to treat bacterial infections dates back to before the time penicillin was discovered. However, the effectiveness of antibiotics led many to ignore the use of bacteriophages. Although antibiotics have many advantages, the problem of bacterial resistance is a significant issue. This is why the world is now revisiting this previously overlooked technology, which has persisted in Eastern European countries. However, the use of phages has yet to be fully integrated and acknowledged on par with antibiotics by the general public.
At The Phage, we are always on the lookout for the latest research updates on phages. As we explore and communicate these developments with the scientific community, we are particularly interested in how phage studies are being applied for the benefit of everyday people. Recently, we discovered something unique: Vitalis Phage Therapy, a phage therapy startup based in India. Among the companies we have spoken with, Vitalis stands out for its distinctive approach to helping patients by providing access to phage therapy in India. This initiative stemmed from the personal experience of the founder, Mr. Pranav Johri.
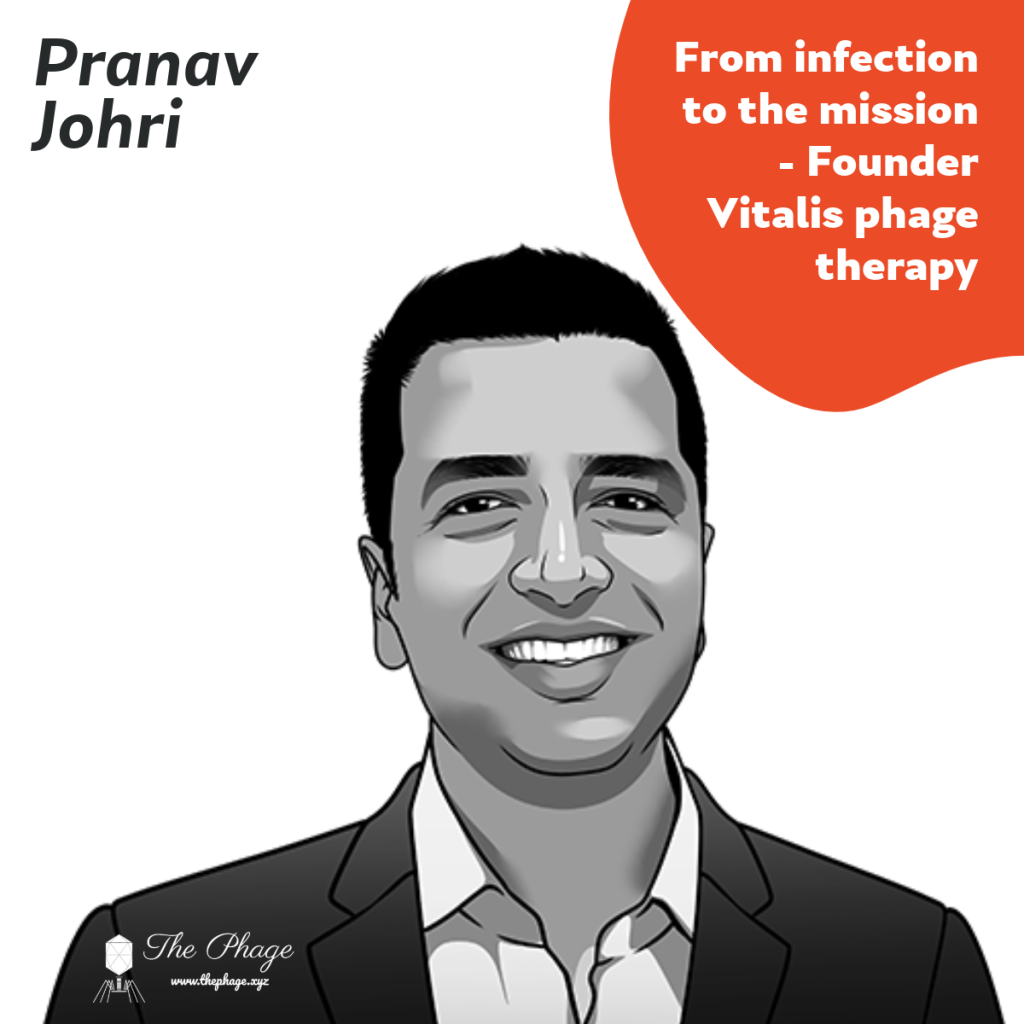
In our interview with Mr Pranav Johri, he shared his personal experience of suffering from recurrent prostatitis and ineffective antibiotic treatments. We reached out to Pranav to hear his story from before he discovered the existence of phages in the era of antibiotic resistance.
Prostatitis involves the inflammation of the prostate tissue and encompasses a wide range of clinical conditions. Men worldwide may struggle with prostatitis at some point in their lives; in fact, it is estimated that approximately 8.2% of men experience prostatitis at some stage. Acute prostatitis and chronic bacterial prostatitis are characterized by documented bacterial infections of the prostate and are typically treated with antibiotic therapy and supportive care.
In 2016, Pranav experienced recurrent episodes of epididymitis and prostatitis, accompanied by repeated bouts of fever. Severe pelvic pain and discomfort led to multiple clinical visits. Despite changes in antibiotic courses, increased dosages, and anti-inflammatory drugs, there was no improvement in his condition. The recurring fever, pain, and discomfort continued unabated.
Despite ongoing treatment efforts, there was no noticeable improvement in his condition, leading doctors to declare the infection to be drug-resistant and eventually give up on further treatment. Pranav was advised to manage his symptoms and accept his condition, resulting in a significantly reduced quality of life.
Disheartened by the lack of progress with antibiotics, Pranav decided to explore alternative solutions for his persistent bacterial infection. Despite the limited literature available at the time, he began researching bacteriophage therapy, which was relatively new and nascent. He reached out to scientists working with phages at research institutions to gain insights into phage research. However, no one he spoke with, had any experience using phage therapy.
Pranav continued his research through medical journals, research papers, and platforms such as Frontiers, PubMed, and NIH. His investigation led him to the Eliava Institute in Georgia, a century-old institution renowned for its work in bacteriophage research and application. When Pranav contacted the institute, his concerns regarding the safety, efficacy, and duration of phage therapy were addressed. With each passing day, he became more convinced that ultimately, phage therapy is the right answer for his condition.
The urologists at the Eliava Institute tested both the prostate fluid and semen (a procedure done for the first time). The results revealed infections with Staphylococcus aureus, Staphylococcus haemolyticus, Streptococcus mitis in the prostate secretion, and Enterococcus faecalis in the semen. Based on these findings, phage therapy was initiated.
The urologists explained to Pranav, why the antibiotic treatments he had previously received were ineffective. He remembers being told that “three main reasons: First, the prostate gland has very little blood flow and an outer membrane that hinders the absorption of antibiotics, meaning only minimal amounts could penetrate the gland. Second, chronic bacterial infections often lead to the formation of bacterial biofilms, which are difficult for antibiotics to penetrate. Third, the bacteria in his condition had developed resistance to the antibiotics he had been prescribed, rendering the repeated doses ineffective”.
Within a week, Pranav noticed an improvement: his low-grade fever disappeared. Over the following weeks, his energy levels improved, though the pain persisted. The infection that had troubled him for months could not be resolved quickly. The doctors reassured him that the pain would gradually diminish over time. Pranav continued with phage medication for the next three months, during which his symptoms and pain progressively improved. However, one pathogen, Streptococcus mitis, remained resistant to the phage strains he was using. The Eliava Institute prepared a custom phage treatment specifically for this pathogen, which ultimately cured Pranav of the remaining infection. Subsequent tests showed that he was finally free of infection.
During this period, Pranav and his wife Apurva, driven by their curiosity, and motivation to provide access to phage therapy to other people suffering with antibiotic-resistant infections, engaged in discussions with doctors and management at the Eliava Institute. They were eager to explore whether phage therapy could be introduced in India, particularly in cases where conventional antibiotics had failed. This became their mission, and in 2018, this vision materialized as the startup “Vitalis Phage Therapy“. Since then, Pranav and Apurva have been spreading awareness about phage therapy across India since then. They have been meeting with medical professionals, newspaper editors, magazine publishers, and various platforms to inform them about the potential of phage therapy for critically ill patients when antibiotics fail. This effort has made phage therapy more accessible to severe cases.

Since 2018, Vitalis Phage Therapy has enabled phage therapy for over 200 patients. One particularly memorable case for Pranav involved a 72-year-old male patient in 2021. After recovering from COVID-19, the patient developed an untreatable hospital-acquired Pseudomonas aeruginosa infection, suffering from urethritis and bloodstream infections in the ICU. Within two weeks of starting phage therapy, the patient was out of the ICU, and by the end of the month, he was fully recovered and discharged from the hospital. This case, among many others, highlights the effectiveness of phage therapy in India.
The mission continues. Today, Vitalis Phage Therapy has established a presence in the Indian medical field, making phage therapy accessible to patients who have not responded to conventional antibiotics. Pranav and Apurva are dedicated to raising awareness among doctors and clinicians through collaborations with hospitals, podcasts, editorials, and research publications. Despite the challenging journey, Vitalis Phage Therapy is fulfilling its mission, truly embodying the Latin meaning of “Vitalis”—”Life.”
After our session with Pranav, we at The Phage, recognized that phage therapy is here to stay and has the potential to integrate into the medical ecosystem. However, much work remains to establish its credibility as a replacement for antibiotics. When asked if phages could replace antibiotics entirely, Pranav responded with a firm “No”. He continues, “Given the extensive scientific foundation and reliance on antibiotics within the medical system, phages would be considered a last resort for infections that cannot be treated with conventional antibiotics. Only when other treatments fail will the medical community turn to phages as an alternative”. Phage research has a long way to go before it could potentially replace antibiotics.